What is Hip Arthroscopy?
Hip Arthroscopy is most commonly performed to treat Femoro-acetabular impingement. In almost every case bone is removed around the hip joint (CAM or Pincer lesions) and the labrum is repaired (or partially removed if irreparable). Many patients will also have some degree of localised cartilage damage and this may either be tidied up (chondroplasty), or a procedure to cover exposed bone is performed (microfracture). I also perform a regenerative procedure to cover exposed bone and replace it with a more cartilage-type material (ABICUS procedure).
What is involved with Hip Arthroscopy?
Specialised equipment is used for hip arthroscopy; the leg is placed in traction and instruments are inserted into the joint to gain access
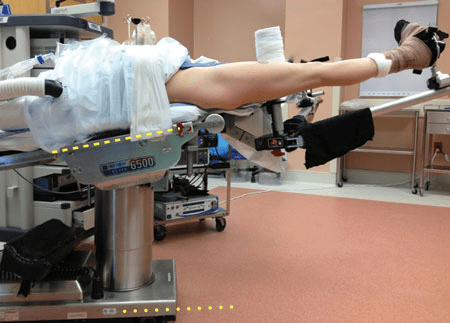
Patient position during hip arthroscopy

Intra-operative View of Hip Arthroscopy
Hip arthroscopy is performed under general anaesthetic (GA). Three small (approx. 10mm) keyhole incisions are made allowing us to pass small camera’s and instruments. Once access is gained, the femoral head and acetabulum (socket) are viewed. The labrum is repaired if necessary.
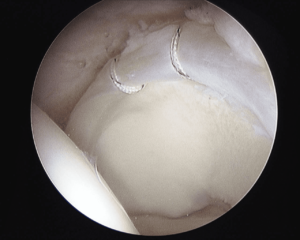
Image showing sutures placed around the labrum following repair.
Once the labrum is repaired any cartilage damage is assessed.
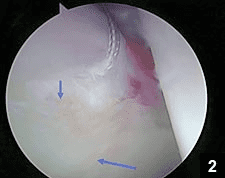
Image showing very minor cartilage damage adjacent to where the labrum has been repaired.
Sometimes the cartilage damage can be severe with a full-thickness defect with underlying exposed bone.
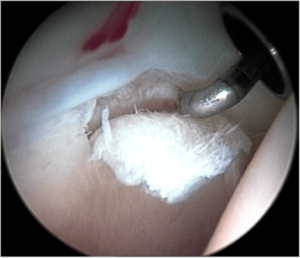
Image showing a chondral flap tear with underlying
In these instances, the tears are trimmed and tidied up and microfracture is performed to stimulate bleeding. This forms a clot and covers the exposed bone with a layer of fibrocartilage.
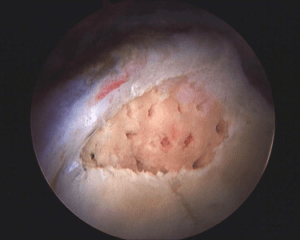
Image showing microfracture
Recovery from Hip Arthroscopy
Although your hip will be sore post surgery, you shouldn’t experience any severe pain. You will be on crutches for 4 – 6 weeks (depending on what exactly was done during the arthroscopy) and won’t be able to drive for this period.
As we do pull on the leg quite hard during the procedure (this is to enable us to get a good look inside the hip joint) there may be some numbness around the groin area but this should resolve in a few days, occasionally weeks.
Good post-operative rehabilitation is key to a good outcome following surgery. Hydrotherapy is very effective in the first few weeks following surgery whilst you are still on crutches. A phased rehabilitation programme is commenced and the full recovery is around 3-6 months.
Complications of Hip Arthroscopy
Hip arthroscopy is a safe procedure with a low complication rate. The overall complication rate is around 4%. Complications include:
- Infection – less than 1 in 1000 (antibiotics are given at the time of surgery to minimise the risk)
- Deep Vein Thrombosis and Pulmonary Embolism (Clots) – rare, less than 1%.
- Nerve Injury – A number of nerves can be damaged as a result of hip arthroscopy and the cause may be pressure on the nerves (lateral femoral cutaneous neve, obturator nerve, pudendal nerve), or excessive traction (femoral and sciatic nerves).
- Vaginal / Perineal Injury / injury to genitalia – May occur from direct pressure causing skin damage.
- Failure to relieve symptoms – Usually due to the presence of arthritis (see outcomes below) or inadequate bone resection.
- Vascular injury – arteries may be damaged as a result of surgery
- Bleeding / Swelling – Bleeding or leakage of fluid may occur for the first few hours after surgery.
- Instability – If too much bone is removed, or too much tissue around the hip (capsular release), the hip can become unstable and sublux or even dislocate.
- Avascular Necrosis of the Hip – If the blood supply of the hip is damaged the ball part of the hip can be affected and die off leading to accelerated arthritis.
- Heterotopic Ossification – sometimes the trauma of surgery causes the tissues around the hip to form bone. This can lead to stiffness.
- Femoral Neck fracture – May occur due to excessive bone removal around the femoral neck.
- Ankle pain – May occur due to tight bandaging around the ankle when applying traction.
Outcome
The main indication for hip arthroscopy is surgery to alleviate femoro-acetabular impingement (FAI). The overall improvement rates for FAI are 80%.
Outcome is influenced by the presence of arthritis, patients with arthritis who undergo hip arthroscopy have an approximate 40% chance of improvement.
Those patients with severe damage at the chondrolabral junction (i.e. localised cartilage damage without widespread arthritis) are more unpredictable in outcome (between 40 and 80% depending on the cartilage damage).